Advances in surgical techniques, such as sinus grafting and implant placement, in conjunction with the advances in restorative materials and techniques, allow patients to regain the aesthetics and function of their original dentition—perhaps even better. The key to the successful and predictable use of advanced surgery and materials is being able to identify the critical diagnostic variables, and to organize them in a manner that will create a treatment plan (and/or alternative plan) that addresses the patient’s chief complaint and dental health. The goal of this article is to assist the dentist in identifying and organizing all the variables of treatment that are responsible for creating predictable outcomes.
 |
 |
|
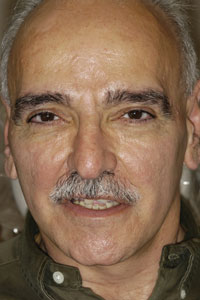
Figure 1. Preoperative full-face view. |
Figure 2. Preoperative smile. |
 |
 |
| Figure 3. Maximum intercuspation. (Note the severe wear). | Figure 4. Protrusive position. |
 |
 |
|
Figure 5. Right-lateral view. |
Figure 6. Left-lateral view. |
 |
 |
|
Figure 7. Mandibular occlusal view. |
Figure 8. Panoramic radiograph. |
 |
 |
|
Figure 9. Cephalometric radiograph. (Note severe cant of the posterior maxillary molars and angle of the occlusal plane). |
Figure 10. Mounted diagnostic casts at the proposed OVD and CR position. (Note the supra-eruption of teeth Nos. 2 and 3 along with the expansion of the right maxillary tuberosity). |
 |
 |
|
Figure 11. Left view of the diagnostic casts demonstrating the supra-eruption of Nos. 14 and 15. |
Figure 12. Left-lateral view showing the mandibular anterior cross section and the anterior angulation of the mandibular incisors. The maxillary occlusal plane has been diagnostically corrected, along with the maxillary incisal edge position. |
 |
|
Figure 13. Anterior diagnostic tooth set-up, done to establish the mandibular incisal edge postion. |
A review of the cephalometric image revealed that the patient exhibited an occlusal vertical dimension (OVD) within normal limits; and this was also clinically demonstrated by examination of his lip support and facial profile, as well as speech evaluation. Though the anterior teeth were significantly shortened, the OVD would not allow for an increase to achieve restoration of the maxillary anterior teeth to proper form and length. Though many times, especially in Class II skeletal relationships, the OVD can be modified to achieve restorative space, an increase was not indicated for this patient. However, the maxillary crown length could be adjusted by repositioning the mandibular incisal position. This could be accomplished th
rough a combination of periodontal crown lengthening, endodontic therapy, and prosthodontic preparation of the teeth to create the required space for the upper teeth. Additional possible therapies would include orthodontic intrusion, orthognathic surgery, or extraction.
Cast modifications and diagnostic waxing were valuable tools used in evaluating the possible treatment options outlined above. For this patient, the first step was to establish an ideal maxillary incisal edge position with a pleasing tooth form and gingival interface. Next, the mandibular incisal edge position was established. A corrected occlusal plane was then created with cast surgery and diagnostic waxing. At this point, the diagnostic work-up revealed that the projected position of the mandibular incisors could not be accomplished with endodontics and periodontal crown lengthening at the proposed occlusal plane. This is extremely valuable information to have prior to beginning any treatment on the patient.
| Table 1. Keys to Diagnostic Records |
|
| Table 2. Parameters of Care |
|
Since a chief goal of the patient was limited treatment time, orthodontic therapy, orthognathic surgery, retention of the mandibular teeth with adjunctive endodontics, and periodontal surgery were eliminated as treatment alternatives. Further diagnostic work was then centered on developing a treatment plan utilizing extraction of the remaining mandibular teeth, alveolar reduction in preparation for immediate implant placement, and temporary restoration (Table 1). To organize all the data obtained from the records, the data was formatted in the Parameters of Care for Partial Edentulism by the American College of Prosthodontists2 (Table 2).
 |
 |
|
Figure 14. One week post operatively. |
Figure 15. Final restorations: anterior view at maximum intercuspation. |
 |
 |
|
Figure 16. Right-lateral view of final restorations. |
Figure 17. Left-lateral view of final restorations. |
 |
 |
|
Figure 18. Occlusal view of the mandibular final restoration. |
Figure 19. Postoperative panoramic radiograph. |
 |
| Figure 20. Final, full-face smile. |
The therapeutic goals were as follows: to aesthetically restore the maxillary anterior teeth to function; to replace the posterior mandibular teeth while restoring function and correcting the occlusal plane; to increase the ability to chew a normal diet; to create an oral environment that minimizes the need for further future restorative care; and to facilitate the ease of oral hygiene procedures.
RISKS, PERFORMANCE ASSESSMENT CRITERIA, AND STANDARD OF CARE
etics and aesthetics would be necessary along with ease of oral hygiene procedures. Finally, patient satisfaction would be vital in achieving success.
PRESENTING THE TREATMENT PLAN TO THE PATIENT
TREATMENT BEGINS: SEQUENCING
PLACEMENT OF FINAL RESTORATIONS: SEQUENCING
At 12 weeks following the surgery, final restorations were accomplished on teeth Nos. 5 to 14 along with the final mandibular restoration. At 16 weeks after sinus grafting, the right maxillary posterior implants were placed in a single-stage protocol. Six months later, final prosthodontic restoration of the right maxillary implants was completed according to the treatment plan. The patient was given a detailed post-treatment maintenance schedule.
SUMMARY
This patient’s treatment involved a complex diagnostic challenge, as well as a challenging clinical sequence due to the utilization of immediate implant placement and restoration after extraction along with immediate prosthodontic restoration with sinus elevation with bone grafting. The inability to have diagnostic patient wax try-ins required a detailed and exacting diagnostic work-up which included significant laboratory diagnostic wax-ups. The utilization of the ACP Parameters of Care for Partial Edentulism for a PDI Class IV patient provided a framework in which care could be planned and executed with confidence. The availability of various reconstructive materials and techniques to create a seamless restorative result is essential to the success of this type of advanced treatment.
References
- American College of Prosthodontists. Parameters of Care for the Specialty of Prosthodontists. J Prosthodont. 2005;14(4 suppl 1):18-25.
- McGarry TJ, Nimmo A, Skiba JF, et al. Classification system for partial edentulism. J Prosthodont. 2002;11:181-193.
- Prosthodontic Diagnostic Index. American College of Prosthodontists Web site.http://www.prosthodon-tics.org/membership/pdi.asp. Accessed October 7, 2008.
- Balshi T, Wolfinger G. Immediate placement and implant loading for expedited patient care: a patient report. Int J Oral Maxillofac Implants. 2002;17:587-592.
Dr. McGarry received his DDS degree in 1975 from UMKC School of Dentistry. He was awarded his certificate in prosthodontics in 1978 from the Veterans Administration Hospital in San Francisco, CA, and became a
Diplomate of the American Board of Prosthodontics in 1991. He is a Fellow in the American College of Prosthodontists and has served as president of the College. He currently holds an appointment as an associate professor at the University of Oklahoma School of Dentistry, and is also an adjunct assistant professor at the University of Illinois School of Dentistry. He maintains a full-time private practice limited to prosthodontics and is the clinical director for the McGarry Implant Institute. He can be reached at mcgarry@implantassociates.net or (405) 755-7777.
Disclosure: Dr. McGarry has no financial interest in any of the companies mentioned in this article.